Diabetes Amputations
How common are diabetes amputations?
The Centers for Disease Control and Prevention (CDC) estimates 23.6 million Americans currently have diabetes. In the past decade, the number of Americans with diabetes has increased heavily from 18.2 million in 2003.
Amputations are a serious concern for people with diabetes. Most amputations are performed on the lower extremities, primarily of the toes and feet. Though it’s less common, some diabetics require amputations below the knee.
Nearly 67 percent of U.S. amputations are linked to diabetes and related complications. According to the CDC, about 73,000 non-traumatic lower-limb amputations were performed in adults aged 20 years or older with diagnosed diabetes in 2010.
An amputation is the surgical removal of a limb or other body part to extract diseased or dead tissue. Depending on the severity and location, an amputation can severely alter personal identity and limit the ability to participate in daily activities. There’s no doubt that people who experience amputations deal with a lot of pain and suffering.
The amputation rate for people with diabetes is 28 times higher than for people without diabetes. Amputations are more common for men than women, with a 50 percent higher amputation rate for male diabetics. The elderly and the non-Hispanic black population are also affected more frequently.
Why do diabetics have a higher risk of amputation?
There are multiple factors that play a role in amputation. Though many of the issues that create cause for an amputation are related to foot care, some are related to glucose management and unknown medication risks.
Nerve damage and poor circulation, worsened by uncontrolled blood sugar, are two major issues that contribute to the need for an amputation. These complications allow infections to set in without a diabetic’s knowledge, causing a gangrenous wound that could later require an amputation.
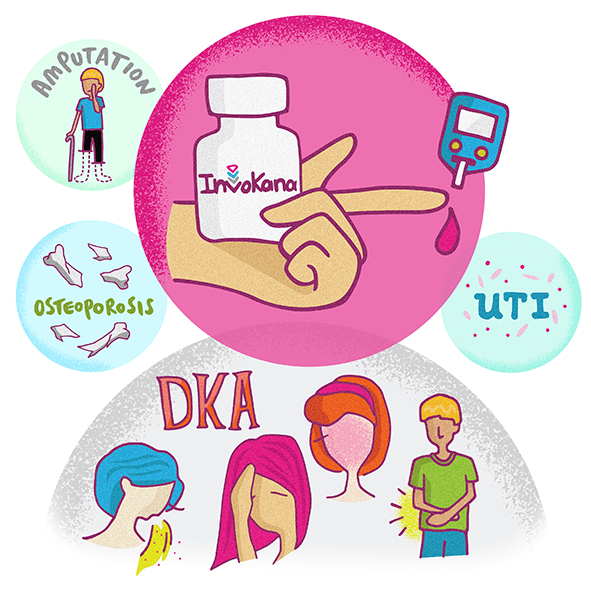
About Invokana and Amputations
Certain medications, such as Invokana, can also increase the risk of amputation. Invokana, the trade name for the drug canagliflozin, is prescribed to patients for the treatment of type 2 diabetes. The drug is licensed from Mitsubishi Tanabe Pharma Corporation to Johnson & Johnson’s Janssen Pharmaceuticals division for distribution throughout most of the world.
According to Janssen Pharmaceuticals, Invokana lowers blood sugar (A1C) and the 300-mg dose is proven to reduce A1C levels more effectively than a competing drug from Merck called Januvia.
What is the reason for the FDA Invokana amputation warning?
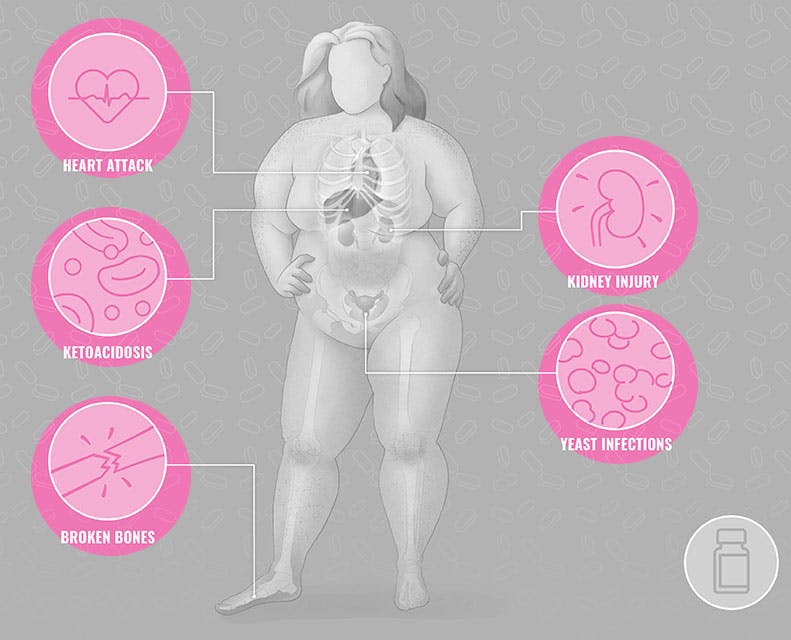
Known Invokana side effects include ketoacidosis, kidney problems, urinary tract infections and a higher risk of broken bones. Amputation risk, however, is a new concern for users of the popular diabetes medication.
In 2017, the U.S. Food and Drug Administration began requiring new ‘black box’ warnings to be added to Invokana labels to describe the increased risk of leg and foot amputations to patients.
The FDA acted following two large clinical trials, CANVAS and CANVAS-R, in which the data demonstrated that leg and foot amputations occurred about twice as often in patients treated with canagliflozin compared to patients treated with a placebo.
What did the Invokana amputation study show?
During the clinical trials, the researchers found that patients most often experienced amputations of the toe and middle of the foot. But, other patients had amputations involving the leg, below and above the knee. In addition, some had more than one amputation and some had both limbs amputated.
One of every 69 patients who take Invokana for five years will have a drug-related amputation.
Despite the increased risk, the trials did not answer the question of why does Invokana cause amputations. According to an article in Forbes, some doctors speculate that while the drug decreases blood sugar and blood pressure, it may also cause the blood to thicken and subsequently pool in the foot.
As researchers struggle to explain why the amputations occur, the FDA did make a note of which types of patients might be predisposed to amputation if they decide to take Invokana. The factors that appeared to increase the odds of amputation included a prior history of amputation, peripheral vascular disease, neuropathy and diabetic foot ulcers.
About SGLT2 Inhibitors and Amputations
Can water pills explain how a certain class of diabetes drugs increase the risk of amputations in people who take the drugs?
That question formed the basis of a new study of type 2 diabetes patients presented last month at the European Association for the Study of Diabetes 2018 Annual Meeting, as Medscape Medical News reported. The study was the latest to investigate the controversy around sodium-glucose cotransporter-2 (SGLT2) inhibitors and an elevated risk of amputation.
SGLT2 inhibitors, prescribed to help lower blood sugar in adults with type 2 diabetes, are sold under the names Invokana, Farxiga and Jardiance. In 2017, more than 2 million people were prescribed SGLT2 inhibitors to manage high blood sugar, as MedTruth noted.
What’s the link between SGLT2 inhibitors and amputation risks?
The SURDIAGENE study followed a large group of type 2 diabetes patients who take water pills. Also called diuretics, these medications work to expel water and salt from the body as urine. The research team found that individuals taking water pills had twice as high a risk of lower limb amputations. They suggest the water pills drained patients’ blood volume, so there was less blood and fluid circulating in the body — what’s known as hypovolemia.
The scientists theorize that this same hypovolemic effect may account for the heightened risk of amputations seen with the SGLT2 inhibitor canagliflozin, or Invokana. In other words, SGLT2 inhibitors could lead to decreased perfusion — the flow of fluid through the bloodstream — particularly in patients who already have poor leg circulation. And that mechanism might explain the increased danger of amputations among people taking SGLT2 inhibitors.
Asked about this theory, Ronan Roussel, MD, PhD, who presented the results and is chief of the endocrinology, diabetes and nutrition department at Group Hôpital Bichat, AP-HP, in Paris, emphasized that the results are "hypothesis-generating," not conclusive. However, he told Medscape Medical News, "If this observation [is accurate], it's probably a class effect.”
And while some scientists pointed to confounding factors — such as heart failure — that might explain the results.
"The hypovolemia hypothesis could provide an explanation for the increased risk of lower limb amputation observed with SLGT2 inhibitors," Roussel nonetheless concluded.
The risk, however, hasn’t been confirmed. Scientists and doctors are working to find more conclusive information about amputation risks and SGLT2 inhibitors.
As scientists continue to investigate these risks, the European Medicines Agency has issued a warning that the entire class of SGLT2 inhibitors for type 2 diabetes may raise the risk for lower-limb amputation. In contrast, the US Food and Drug Administration has limited its advisory to one SGLT2 inhibitor — Invokana. However, in September, the agency issued a new safety announcement, warning of a potential link between a rare, destructive bacterial infection and diabetes drugs like Invokana, Farxiga and Jardiance.
What are the amputation risks with Invokana, Farxiga and Jardiance?
In July, new research published in the peer-reviewed journal Diabetes, Obesity & Metabolism attempted to get to the bottom of the risks around the entire class of SGLT2 inhibitors. The study found a higher rate of amputations among all SGLT2i patients, including individuals taking the SGLT2 inhibitors Farxiga (dapagliflozin) or Jardiance (empagliflozin). The heightened risk, however, was not statistically significant.
More recently, a research team in Australia followed a small group of type 2 diabetes patients with open foot wounds, which puts them at greater risk for amputations. One group was taking Farxiga or Jardiance, while a control group of patients was not. Researchers found amputations occurred in both groups, but the control group had a higher rate of amputations (0.60 amputations in the control group compared to 0.41 in the group taking SGLT2 inhibitors), according to the paper published in September in the Journal of Clinical and Translational Endocrinology.
“This study is therefore the first to provide real-world data on the use of SGLT2i in patients with open foot wounds and offers some reassurance on the use of empagliflozin and dapagliflozin in people at high risk of amputation," the authors noted.
Still, the small size of the study, and conflicting results on the risks of SGLT2 inhibitors, suggests more work needs to be done to help diabetes patients navigate their risks.
How to Prevent Diabetic Amputations
What are the risk factors for diabetic amputations?
Diabetics have sensitive feet that are more vulnerable to injuries, especially when blood glucose in unmanaged. All of the factors that lead to amputations actually work together, so it’s important to be aware of each one.
Diabetic neuropathy reduces sensation, making patients unaware they have injuries because they can’t feel wounds developing. Poor circulation, on the other hand, keeps injuries from healing properly. Knowing the risk factors for diabetic amputation are key to prevention.
Diabetic Neuropathy
Diabetic neuropathy, a common diabetes complication, is a form of nerve damage caused by high blood sugar. It injures nerve fibers throughout the body, leaving patients with decreased feelings in the lower limbs and feet. Because of neuropathy, diabetics may not feel hot or cold temperatures. They might not notice a cut or callous that makes them more vulnerable to infection.
“You could have a tack or stone in your shoe and walk on it all day without knowing. You could get a blister and not feel it. You might not notice a foot injury until the skin "breaks down and becomes infected.”
American Diabetes Association
There are four types of diabetic neuropathy: peripheral neuropathy, autonomic neuropathy, radiculoplexus neuropathy and mononeuropathy. Symptoms of diabetic neuropathy might include pain, numbness, tingling, burning. For some people with neuropathy, digestive issues, bladder problems, vision complications, erectile dysfunction are experienced.
Poor Circulation
Diabetes may affect blood vessels, causing them to narrow, harden. This limits blood flow to the legs and feet. A lack of blood flow can affect the ability to fight infections in addition to slowing the speed of wound healing. Some identifiable indicators of poor circulation include peripheral vascular and arterial disease.
Smoking also affects the small blood vessels in the body. Smoking can reduce blood flow throughout the limbs, and it makes injuries harder to heal. Many diabetes who require amputations are smokers.
Skin Changes, Calluses, Ulcers
Skin changes, related to nerve damage, affects the natural oils and moisture in the feet. When diabetes affects the skin of the feet and toes, it causes dryness. Dryness makes the skin more likely to peel and crack. If the natural regulatory state of the foot changes, it makes the patient more vulnerable to injury, infection and amputation.
Calluses, caused by repeated friction, pressure or irritation, are also more common with diabetes. Untrimmed and untreated calluses can cause complications, which frequently occur on the ball of the foot or on the bottom of the big toe. Calluses may develop into ulcers, which are painful open sores.
Neglecting or walking on ulcers can result in deeply embedded infections. Many of these wounds are non-healing, which may lead to the loss of a limb.
Invokana
People with diabetes are already at a higher risk of amputation, but studies show the popular medication Invokana can double the risk. The reason for an Invokana amputation is not yet clearly understood. However, researchers confirm that Invokana in conjunction with other risk factors makes amputation more likely.
A history of prior amputation may also predispose patients taking Invokana to the need for amputation. Patients with a history of amputation or peripheral vascular disease had the highest amputation risk, but the relative risk was similar. Regardless of a prior risk, diabetic patients are encouraged to talk to their doctors about the potential amputation side effects of Invokana.
Most diabetic foot infections require some surgical intervention, but many foot problems are actually avoidable. It’s possible to prevent diabetic foot ulcers and amputations by understanding the risk factors, key elements of proper care and any and all medication risks upfront.